Hemispherectomy And The Time After The Operation
A hemispherectomy is a surgical procedure used to treat various disorders that cause seizures. Usually, doctors perform it when these disorders do not respond adequately to other, less radical treatments.
The first hemispherectomy was performed on a dog in 1888. The first evidence that this procedure was performed on humans dates back to 1923. In the 1960s and 1970s, several of the procedures performed poorly.
These days, things have changed. Doctors often choose an anatomical hemispherectomy instead of a functional hemispherectomy. This is a more accurate and less invasive procedure. The success rate is much higher than in the past.
In this article, we will take a closer look at the modern forms of this procedure.
What is a hemispherectomy?

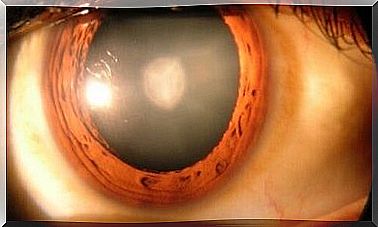
A hemispherectomy is a neurosurgical procedure that involves removing one of the hemispheres of the brain.
Sometimes the surgeon removes the left hemisphere of the brain. Other times, they remove the right hemisphere. Doctors mainly perform this procedure in extreme cases and on children between 5 and 10 years.
This type of intervention is essentially an anticonvulsant treatment. However, it is also useful for patients with neurological deficits and in severe cases of severe head trauma.
In most procedures, the entire brain half is removed. Sometimes, however, only part of it is removed. This is called a functional hemispherectomy. In such cases, if doctors leave a small part of the damaged tissue, the seizure-causing disorder may reappear.
When is this procedure performed?
In general, medical professionals can recommend a hemisphericectomy to patients suffering from continuous and daily seizures who have not responded to other medical treatments or other less invasive surgical procedures.
Medical professionals recommend it in the following cases:
- Children with hemiplegia. This is only for children over the age of four who suffer from seizures and / or mental disorders, and after following for two years that the patient has not responded to medical treatment.
- Sturge-Weber syndrome. This is a neurocutaneous disorder characterized by a birthmark on the face around the trigeminal nerve area. Doctors may recommend this type of surgery when crises begin at an early age and the disorder affects the entire hemisphere.
- Rasmussen’s encephalitis. This brain disorder causes chronic, progressive encephalitis. It is best to have the procedure performed early.
- Hemimegalencephaly (HME). This is a rare inflammatory neurological disease that causes severe seizures. Medical personnel still do not agree that surgery is in fact the best option for patients suffering from this disorder.
- Malformations in cortical development.
Characteristics of the procedure
In all, there are four types of hemispherectomy.
The four types are:
- Anatomical hemispherectomy
- Hemidecortication
- Functional hemispherectomy
- Modified functional hemispherectomy
Doctors usually use anesthesia for the procedure.
The surgeon starts by shaving the patient’s head and marking where it should be cut. Then it is cut to expose the dura mater. Then it is removed so that one can reach the brain.
Furthermore, they carefully mark the area they need to remove. They do so, and cauterize the blood vessels. They place a drainage device. Finally, they place the dura feeder and scalp back, and close the incision with pins.
The period after a hemispherectomy operation
Unfortunately, the period after this procedure is painful.
Usually doctors leave the drainage pipe for 3 to 4 days. After that, the patient is assessed and it is decided whether they should remove it or not. Before removing it, however, they must perform diagnostic tests to determine if there is bleeding.
Seizures during the period after the procedure are another serious complication. About half of the patients usually develop hydrocephalus. At the same time, almost all patients develop aseptic meningitis.
There is also evidence that some complications may manifest later.
Nevertheless, the mortality rate is quite low, at between 4% and 6%.